Current Projects
MetaSurg
The MetaSurg-Gehirn study investigates the effects of gastric bypass surgery on brain anatomy. Our sample consists of participants of Prof. Dietrichs Meta-Surg study at the University Clinical Centre in Leipzig. The participants undergo magnetic resonance imaging (MRI) at the beginning of participation and 6 and 12 months after surgery. Additionally, participants complete a computer-based test of cognitive performance as well as behaviour questionnaires.
GutBrain
How are food decisions determined? Which role does plays the gut microbiome play in food decision-making? Can a high-fiber diet (representative of a reflecting fiber intake of a plant-based diet) change the gut microbiome and in turn change food wanting / food decisions? Does reward-related Changes the BOLD activation of the brain‘s reward areas after a fiber intervention change? Which role does plays food wanting play in food recognition memory? Does the white matter pathway connecting reward and memory areas (the uncinate fasciculus) determine food memory or the interplay of food wanting and food memory? Does hunger enhance food recognition?
These and many more questions are answered by the results of the GutBrain-Study, a randomized placebo-controlled within-subject crossover intervention study with 60 healthy, overweight, omnivorous adults in two arms: high-fiber vs placebo intervention for 14 days. Participants underwent extensive testing on four test days including two 3T-fMRI tasks, structural and diffusion-weighted MR brain imaging; they provided blood and stool samples and took part in a computer-based attention task as well as in questionnaires.
MIFOOD
MIFOOD project aims to study the gut-brain axis. The stability and functionality of this axis can be affected by psychological or gut-directed (e.g., food, medicine, infection) distresses. Therefore, we are planning to modulate gut-brain communication through a prebiotic diet and neurocognitive behavioral lifestyle intervention (NCBL), respectively, which will enable us to discover microbiota communities and brain regions playing a key role in eating behavior.
For this purpose, a total of 90 people with overweight/obesity, defined as BMI >=25 kg/m2 between the age of 18 and 60 years are being recruited. After signing the consent form, eligible participants undergo baseline assessments which they are asked to refrain from eating for at least 12 hours overnight. First, a blood sample is taken from participants in the fasting state to obtain metabolic markers. Then, body fat and anthropometrics are measured. Next, they receive a light breakfast with 10% of their individual need. Subsequently, participants undergo task-based fMRI and additional other MRI sequences. Questionnaires are filled at site and online. After baseline assessments, a 6-month intervention takes places where participants are randomly divided into three parallel arms: prebiotics (30mg per day), NCBL intervention, and control (supplementary placebo) groups. Subsequently, a follow-up assessment occurs.
This project is ongoing, if you are interested, you can contact mi-food@cbs.mpg.de.
LongCovid
COVID-induced neurological changes are often investigated in samples of severe, acute patients. In this study, we acquire anatomical images from participants with long COVID and analyse the data in combination with previous scans from the LIFE study. We further investigate a possible connection of brain changes to functions commonly affected in long COVID like memory or olfaction.
In a further study in collaboration with the Clinic for Cognitive Neurology at Leipzig University Clinical Center, we aim to assess neurological and cognitive effects of a neuro-psychotherapeutic intervention program in patients with post-COVID.
Preventive options for healthy aging
In first interventional studies, we and others showed the potential of dietary factors, including caloric restriction, polyphenols and omega-3 fatty acids, for improving cognitive functions and AD-related brain structures in older humans, possibly via improvements in metabolic and inflammatory markers. However, another study of our group could not confirm results for supplementary resveratrol, challenging the hypothesis that a single nutrient exerts influence when not tightly controlling further lifestyle-related behaviours. To address this issue more comprehensively, we are now testing if a multi-component lifestyle intervention, compared to clinical routine, exerts synergistic effects on brain structure and cognition in an ongoing long-term multi-center trial (AgeWell.de).
Further topics
Genetic determinants of obesity
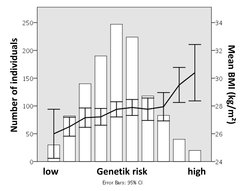
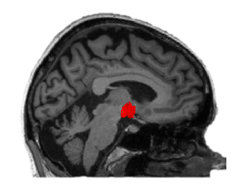
Within the framework of the CRC Obesity Mechanisms of the University of Leipzig we explore the influence of genetic factors on obesity-related behaviours, such as unhealthy and compulsive eating traits, and their neuronal correlates using high-resolution magnetic resonance imaging (MRI) in a population-based sample - the Health Study of the Leipzig Research Center for Civilization Diseases (LIFE)-cohort. To further increase statistical power, we initiated meta-analyses in the international NeuroCHARGE-consortium. Preliminary results indicate that hypothalamus microstructure predicted variance in body mass index (BMI), and genetic underpinnings of this phenotype would now allow us to characterize possible mechanistic pathways.
Eating behaviour
Besides genetic factors, our "obesogenic environment", i.e., abundance of cheap high-caloric food together with low physical activity demands at work and in leisure times, promotes weight gain. Here, the inability to control hedonic eating and avoid unhealthy food refrains from maintaining a normal weight, and intriguingly, recent studies propose that the food that we consume could also change subsequent decision-making. We thus aim to explore the complex interplay between homeostasis-regulating brain centers, cognitive control of impulsivity and reward tendencies, as well as nutrient signalling in determining every-day eating behaviour and obesity.
Dietary impact
Studies in patients undergoing bariatric surgery indicated that food reward evaluation normalized after surgery. Yet, how dietary changes induce plasticity in the human brain that leads to healthier food choices and better cognition remains to be fully understood. In a study evaluating alternative eating habits such as vegetarian and vegan diets, we study the possibility that a plant-based diet, possibly via changes in the metabolism and microbiota composition, changes the neuronal processing of food preference and further psychological measures such as mood and well-being. While clarifying if a potentially both environmentally and economically friendly eating pattern impacts cognitive processes, our study might help to get a better mechanistic understanding of gut-body-brain interactions.
Detrimental consequences of obesity

On the long run, overeating and obesity affect brain structure and function via co-morbidities such as hypertension and type 2 diabetes. Also, excess of inflammatory cytokines and adipokines by adipose tissue is detrimental for the brain. It has been shown that even in the absence of manifest obesity, better metabolic profiles exert protective effects on Alzheimer’s disease (AD) risk and might protect AD-related brain areas. In the LIFE-study, our group revealed that a higher BMI and more so visceral fat is linked with white matter lesions and gray matter reductions in the aging population even after controlling for confounders, and lower grey matter volume for example in prefrontal areas also mediated the negative effect of higher age and higher BMI on memory. We were further able to show that higher BMI is associated with reduced connectivity in the default mode network, a finding that may reflect a predisposition to AD.


